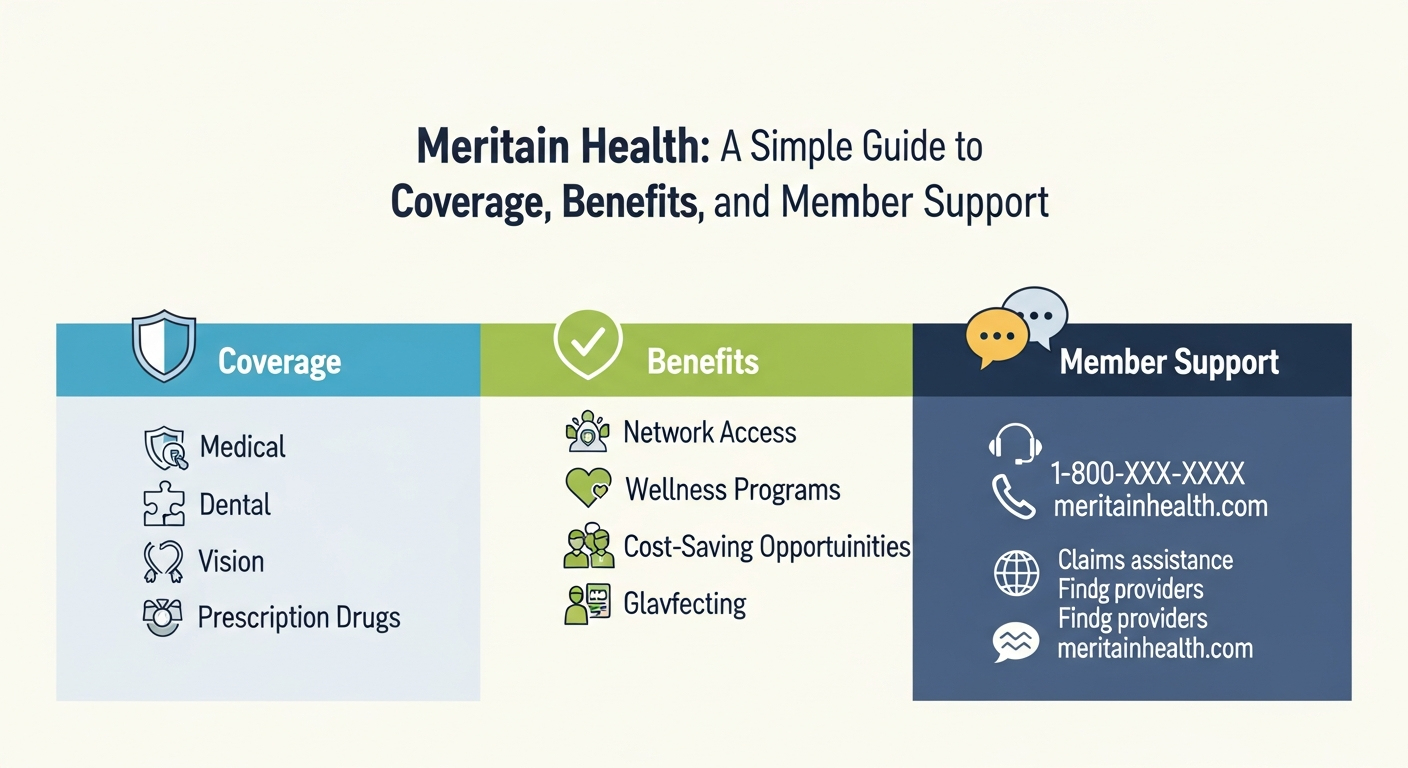
Meritain Health: A Simple Guide to Coverage, Benefits, and Member Support
Health insurance can feel confusing. Many people feel lost when choosing a plan or filing a claim. That is where Meritain Health comes in. Meritain Health helps employers and members manage healthcare benefits in a clear and organized way. It focuses on making healthcare easier to understand and easier to use.
Meritain Health works mainly with employer-sponsored health plans. Instead of selling insurance directly, it helps manage benefits, claims, and networks. This approach gives employers more control and members better support. Over the years, Meritain Health has built trust by offering reliable service and simple tools.
In this guide, we will explain what Meritain Health is, how it works, and why many employers choose it. You will also learn about plans, provider networks, claims, and customer support. Everything is explained in simple words, so anyone can understand it.
What Is Meritain Health?
Meritain Health is a health benefits administrator. This means it helps manage health plans for employers. It does not sell insurance like traditional insurance companies. Instead, it supports self-funded and employer-based health plans.
Meritain Health is part of the Aetna family. This connection gives members access to strong provider networks and trusted healthcare resources. Employers choose Meritain Health because it offers flexibility and cost control. Members like it because services are easy to use and clearly explained.
The company focuses on handling claims, managing networks, and supporting members. It also provides tools to help people understand their benefits. Meritain Health aims to reduce stress and confusion around healthcare.
By combining experience and technology, Meritain Health creates a smooth healthcare experience. This balance helps both employers and members feel confident and supported.
How Meritain Health Works for Employers
Meritain Health supports employers who want more control over healthcare costs. Many companies use self-funded plans. In these plans, employers pay for employee healthcare directly. Meritain Health helps manage these plans smoothly.
The company handles claims processing, customer service, and provider networks. This saves employers time and effort. Employers also receive detailed reports that help track healthcare spending.
Meritain Health offers flexible plan design. Employers can choose coverage options that fit their workforce. This customization helps control costs while still supporting employee health.
With strong data and clear reporting, Meritain Health helps employers make smarter decisions. This approach builds trust and long-term partnerships.
Meritain Health Plans and Coverage Options
Meritain Health supports many plan types. These include PPO plans, high-deductible health plans, and customized employer plans. Coverage depends on what the employer chooses.
Most Meritain Health plans include doctor visits, hospital care, and preventive services. Some plans also include mental health and wellness programs. Prescription drug coverage is often included through partner networks.
Members can review their plan details online. This helps them understand what is covered and what costs to expect. Clear information helps members make better healthcare choices.
Meritain Health focuses on flexibility. This allows employers to offer benefits that match employee needs.
Provider Networks Used by Meritain Health
Meritain Health uses strong provider networks. Many plans use the Aetna network. This gives members access to a large number of doctors and hospitals.
Using an in-network provider usually lowers costs. Meritain Health makes it easy to search for providers online. Members can check if a doctor or hospital is covered before getting care.
Out-of-network coverage may be available, depending on the plan. Members should always review their benefits first. This helps avoid surprise bills.
Strong networks are a major reason people trust Meritain Health.
Claims Processing With Meritain Health
Claims processing is one of Meritain Health’s main services. After a medical visit, the provider sends a claim to Meritain Health. The company reviews the claim and applies plan rules.
Meritain Health aims to process claims quickly and accurately. Members can track claims online. This transparency builds trust and reduces confusion.
If a claim is denied, members can review the explanation. Appeals are available if something seems wrong. Customer support can help explain next steps.
Clear claims handling is a key strength of Meritain Health.
Meritain Health Member Portal and Tools
Meritain Health offers an online member portal. This portal helps members manage their benefits easily. Users can view claims, check coverage, and download ID cards.
The portal also shows deductible and out-of-pocket balances. This helps members plan healthcare expenses. Clear visuals make information easy to understand.
Some plans include wellness tools and health resources. These tools support better health decisions. They also encourage preventive care.
Easy digital access improves the overall member experience.
Customer Support and Member Experience
Customer service matters in healthcare. Meritain Health offers phone and online support. Representatives help answer benefit questions and explain claims.
Many members appreciate the clear communication. Simple explanations reduce stress. This is important during medical situations.
Support teams are trained to handle complex issues. They aim to resolve problems quickly. This builds confidence and trust.
Good support is a major reason employers choose Meritain Health.
Meritain Health and Aetna: The Connection
Meritain Health is part of Aetna, one of the largest healthcare companies in the U.S. This relationship strengthens its services.
Through Aetna, Meritain Health members often access large provider networks. This means more choices for care. It also improves nationwide coverage.
Aetna’s experience adds authority and reliability. This partnership supports Meritain Health’s long-term success.
Together, they offer strong healthcare solutions.
Who Should Choose Meritain Health?
Meritain Health is ideal for employers wanting flexible benefits. It works well for mid-size and large companies. Self-funded plans benefit most from its services.
Employees who want clear tools and support also benefit. Simple portals and helpful staff improve the experience.
If you value transparency and flexibility, Meritain Health is a strong option. It balances cost control with member care.
Choosing the right administrator can improve healthcare satisfaction.
FAQs About Meritain Health
Is Meritain Health an insurance company?
No. Meritain Health manages health plans but does not sell insurance directly.
Does Meritain Health use the Aetna network?
Yes. Many Meritain Health plans use the Aetna provider network.
How do I check my Meritain Health benefits?
You can log into the Meritain Health member portal to view plan details.
Can I see any doctor with Meritain Health?
It depends on your plan. In-network doctors usually cost less.
How long do claims take to process?
Most claims are processed quickly. You can track progress online.
Does Meritain Health offer customer support?
Yes. Members can get help by phone or online support tools.
Final Thoughts on Meritain Health
Meritain Health plays an important role in employer healthcare plans. It focuses on clarity, flexibility, and support. By managing claims and networks, it helps both employers and members.
The connection with Aetna adds strength and reliability. Easy tools and strong customer service improve trust. For many organizations, Meritain Health offers a smart balance between cost control and care quality.
If you want a health benefits partner that values simplicity and transparency, Meritain Health is worth considering. Explore your plan details and use the tools provided to get the most from your coverage.